Pain is something we all know intimately — a stubbed toe, a headache that ruins your day, the deep ache of a long-term condition. Yet despite its universality, pain remains mysterious: why two people feel the same injury so differently, why stress makes it worse, or why sometimes pain lingers long after an injury has healed. In this article we’ll take a tour from the skin’s nerve endings up to the highest regions of the brain, exploring how pain signals begin, travel, change, and are finally interpreted. You’ll gain a practical understanding of the biology, the psychology, and the treatments that shape the way pain is experienced. Along the way I’ll share surprising facts and simple analogies to make the neuroscience feel relevant and human.
Содержание
What Is Pain? More Than a Signal
Pain is often defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage. That phrase matters: pain is not simply raw information about harm; it’s a complex mix of sensory input and emotional interpretation. Imagine pain as a movie rather than a photograph. The initial frame — the injury — sets the scene, but the script, the lighting, the music, and the audience’s expectations all determine how the movie feels to you. That’s why pain includes sensations (sharp, burning, aching), but also emotions (fear, annoyance), thoughts (what will happen next?), and behaviors (withdraw, guard, seek help).
People use the word pain to mean different things. Clinicians distinguish types such as acute pain (short-lived, usually linked to clear tissue damage) and chronic pain (persistent, lasting months or more, often with complex causes). Understanding these types helps explain why treatments that work for one form of pain may fail for another.
From Stimulus to Signal: How Nerves Detect Danger
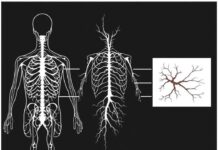
Every pain story starts at the periphery with specialized sensors called nociceptors. These are nerve endings embedded in skin, joints, muscles, and internal organs. They respond to noxious mechanical forces, extreme temperatures, and chemical irritants released by injured tissues.
Types of Nociceptors
Nociceptors are diverse. Some respond to mechanical injury (cut, pinch), others to thermal extremes (hot, cold), and some to chemical changes (acid, inflammatory mediators). Their diversity helps the nervous system distinguish different kinds of threats.
- Polymodal nociceptors: respond to multiple types of painful stimuli.
- Silent nociceptors: normally inactive but become responsive after inflammation.
- Visceral nociceptors: detect pain in internal organs and often produce poorly localized, aching pain.
When nociceptors are activated, they convert mechanical, thermal or chemical energy into electrical signals — a process called transduction. These signals travel along peripheral nerve fibers toward the spinal cord.
Fast and Slow: A-delta and C fibers
Not all pain travels at the same speed. Two main fiber types carry nociceptive information to the spinal cord:
| Fiber Type | Speed | Sensation | Myelination |
|---|---|---|---|
| A-delta | Fast (5–30 m/s) | Sharp, well-localized initial pain | Thinly myelinated |
| C fibers | Slow (0.5–2 m/s) | Dull, burning, aching, lingering pain | Unmyelinated |
That classic two-stage pain — first a sharp jab, then a throbbing ache — reflects the different timing of these fibers. The signals enter the spinal cord and make their first major synapse in the dorsal horn.
The Spinal Cord: First Stop for Pain Processing
The spinal cord is not a simple relay station; it’s an active processor. In the dorsal horn (the back part of the spinal cord), incoming nociceptive fibers connect with second-order neurons that send information up to the brain. But they also interact with local interneurons that can amplify or dampen the signal.
Gate Control Theory in Plain English
In the 1960s, the gate control theory proposed that the spinal cord contains a “gate” that can increase or decrease transmission of pain signals to the brain. While the original model was simplified, it captures an important truth: non-painful input (like rubbing your skin) can reduce pain, and the spinal cord’s circuitry can be modulated by both peripheral input and descending commands from the brain.
Think of the dorsal horn as a crowded door. A-delta and C fibers push to get through, but touch fibers and inhibitory interneurons can hold the door partially closed. Descending signals from the brain act like supervisors who can tell the doorkeepers to open or shut the gate depending on the context.
Neurochemistry in the Spinal Cord
At synapses in the dorsal horn, chemical messengers determine whether an incoming signal will be transmitted upward. Important players include:
- Glutamate — the main excitatory neurotransmitter that amplifies pain signals.
- Substance P and CGRP — neuropeptides released by nociceptors that promote inflammation and sensitization.
- GABA and glycine — inhibitory transmitters that reduce signal transmission.
- Endogenous opioids — enkephalins and endorphins that suppress pain at the spinal level.
When injury or inflammation occurs, this balance can shift toward excitation, producing heightened sensitivity or allodynia — pain from normally non-painful stimuli.
Upward to the Brain: Where Pain Becomes Experience
Signals that pass the spinal gate travel up the spinal cord in pathways like the spinothalamic tract to reach brain regions that create the conscious experience of pain. The brain doesn’t have a single “pain center.” Instead, it uses a network often called the “pain matrix,” including the thalamus, primary and secondary somatosensory cortices, insula, anterior cingulate cortex (ACC), prefrontal cortex, and limbic structures.
Key Brain Regions
- Thalamus — a relay station that distributes sensory information.
- Somatosensory cortices (S1 and S2) — process the sensory-discriminative aspects: location, intensity, quality.
- Insula — integrates interoceptive sensations and contributes to the subjective feeling of pain.
- Anterior cingulate cortex (ACC) — linked to the emotional and motivational aspects, such as unpleasantness and attention to pain.
- Prefrontal cortex — involved in evaluation, expectation, and decision-making about pain.
- Amygdala and hippocampus — connect pain to fear, memory, and learning.
Together these regions answer questions such as: Where is the pain? How bad is it? How concerned should I be? What should I do?
Context Shapes Pain
One of the most striking findings in pain science is that the brain’s interpretation of signals is heavily influenced by context. Expectation, attention, mood, and previous experiences all shape how pain is perceived. If you expect intense pain, pain often increases; if you are distracted or reassured, it may decrease. This is where placebo and nocebo effects come in — beliefs and suggestions can powerfully change pain by engaging endogenous modulatory systems.
Plasticity: When Pain Learns and Changes the Nervous System
Neuroscience has shown that the nervous system is plastic — it changes with activity. In the context of pain, plasticity can be adaptive (helpful healing responses) or maladaptive (leading to chronic pain). After injury, peripheral nerves and spinal circuits may become sensitized: their thresholds lower and they respond more strongly. In the brain, circuits involved in pain, emotion, and memory can reorganize, reinforcing pain pathways and making pain more likely to persist.
Central sensitization is a key concept: it describes a state where the central nervous system is in a persistent state of high reactivity. Clinically, central sensitization can explain widespread pain, disproportionate pain responses, and sensitivity to non-painful stimuli.
Examples of Maladaptive Changes
- Phantom limb pain: after amputation, the brain’s body map reorganizes and can produce vivid pain in a missing limb.
- Fibromyalgia: widespread pain with central sensitization and altered pain modulation.
- Chronic low back pain: altered cortical processing and emotional circuitry contribute to persistent suffering even after tissue healing.
Recognizing plasticity gives hope: if circuits change for the worse, they can also be retrained or modulated for improvement.
The Role of Emotions, Attention, and Memory
If you’ve ever noticed pain feeling worse when you’re stressed or distracted, you’ve observed how psychology affects pain. Stress and negative emotions can amplify pain through hormonal and neural pathways (e.g., cortisol, increased sympathetic activity). Conversely, positive emotions, social support, and effective coping strategies reduce pain’s impact.
Attention is a powerful modulator. When you focus intently on a painful stimulus it often feels stronger. Athletes sometimes report reduced pain during competition because of intense focus and strong motivation.
Memory and learning shape expectations. If a treatment worked before, your brain might expect relief and engage endogenous pain relief systems; if a prior experience was traumatic, the brain may anticipate intense pain and amplify signals.
Neurochemistry and Pain: A Quick Guide
Understanding pain also means knowing the chemical messengers that influence it. Here is a simple table to summarize some major players:
| Neurochemical | Primary Role in Pain |
|---|---|
| Glutamate | Main excitatory transmitter in nociceptive synapses; key in sensitization |
| Substance P / CGRP | Neuropeptides that enhance pain signaling and inflammation |
| GABA / Glycine | Major inhibitory transmitters that suppress pain transmission |
| Endogenous opioids (endorphins, enkephalins) | Natural pain-relieving peptides acting at spinal and brain opioid receptors |
| Serotonin / Norepinephrine | Involved in descending pain modulation; target of some antidepressants used for pain |
| Endocannabinoids | Modulate synaptic transmission and reduce pain signaling |
Drugs that target these systems form the backbone of many pain treatments, and emerging therapies aim to tune these chemicals more precisely.
Assessing Pain: How Clinicians Listen
Because pain is subjective, clinicians rely on structured assessments: history, physical exam, and validated scales. Common tools include the Numeric Rating Scale (0–10), Visual Analog Scale, and questionnaires that probe function, mood, and sleep.
A thorough pain assessment asks not only “how bad?” but also “what does it stop you from doing?” and “what makes it better or worse?” Understanding pain’s context, timing, and associated symptoms helps distinguish nociceptive pain (linked to tissue damage), neuropathic pain (from damaged nerves), inflammatory pain, and centralized pain.
Treatments: A Toolbox, Not a Single Cure
Because pain is complex, treatments must be too. Effective care often combines medications, procedural interventions, physical rehabilitation, and psychological strategies. Here’s a practical overview.
Medications
- Analgesics: acetaminophen and NSAIDs for mild-to-moderate nociceptive pain.
- Opioids: potent analgesics for acute severe pain or uncontrolled cancer pain; risks and long-term effectiveness for chronic noncancer pain are debated.
- Antidepressants (e.g., SNRIs, TCAs): useful for neuropathic pain and conditions with central sensitization.
- Anticonvulsants (gabapentin, pregabalin): help neuropathic pain by stabilizing hyperexcitable nerves.
- Topicals (lidocaine, capsaicin): useful for localized neuropathic pain.
Interventional and Procedural Options
Nerve blocks, epidural injections, radiofrequency ablation, and spinal cord stimulation are options when conservative measures fail. They can be effective for certain conditions but require careful patient selection.
Physical and Occupational Therapy
Movement matters. Graded activity, strengthening, and retraining movement patterns can reduce pain and improve function. Physical therapy also reduces fear of movement and helps in retraining the nervous system.
Psychological Therapies
Cognitive-behavioral therapy (CBT), acceptance and commitment therapy (ACT), and mindfulness-based approaches help patients change their relationship to pain. These therapies are evidence-based and can reduce pain-related disability by addressing thoughts, emotions, and behaviors.
Complementary Approaches
Acupuncture, massage, yoga, and tai chi provide benefit for some people, often by reducing stress, improving mobility, and engaging endogenous pain-modulating systems. Evidence varies by modality and condition.
Emerging and Cutting-Edge Treatments
Science keeps advancing. Neuromodulation techniques (transcranial magnetic stimulation, deep brain stimulation), gene therapy, targeted monoclonal antibodies (e.g., against CGRP in migraine), and virtual reality for pain distraction are promising areas. Personalized medicine, where treatments are chosen based on genetic and neurobiological markers, is an exciting horizon but not yet commonplace.
Practical Tips for Living with Pain
If you or someone you care for lives with persistent pain, these practical approaches can help reduce suffering and reclaim life:
- Keep moving within limits: graded activity can prevent deconditioning and reduce fear.
- Use a multi-pronged plan: combine physical, medical, and psychological strategies.
- Address sleep and mood: poor sleep and depression amplify pain sensitivity.
- Learn pacing: balance activity and rest to avoid flare-ups.
- Practice relaxation and mindfulness: they lower stress and modulate brain circuits.
- Communicate clearly with clinicians: describe how pain affects daily life, not just intensity.
Special Populations and Considerations
Pain in children, older adults, and people with cognitive impairment requires tailored approaches. Children may express pain differently and need age-appropriate assessments. Older adults often have multiple comorbidities and polypharmacy risks, so treatments must be chosen carefully. Cultural background also affects pain expression and treatment preferences.
Common Myths and Misconceptions
People often believe myths that can hinder care. Let’s debunk a few:
- Myth: If pain lasts long, it means there’s ongoing tissue damage. Reality: chronic pain can persist after tissues heal due to nervous system changes.
- Myth: Opioids are the best long-term solution for chronic pain. Reality: opioids may help short-term but carry risks and limited long-term benefits for many chronic conditions.
- Myth: Pain is “all in your head.” Reality: pain always involves the brain, but that doesn’t mean it’s imaginary or under voluntary control.
Understanding these facts empowers patients and clinicians to make better choices.
How to Talk About Pain
Words matter. Describing pain using sensory and emotional details helps clinicians pick appropriate treatments. Instead of only saying “it hurts,” try: “It’s a burning, constant ache that worsens when I stand for long and makes it hard to sleep.” That gives actionable clues.
Prevention: Can We Reduce Future Pain?
While not all pain is preventable, many strategies lower risk:
- Practice safe body mechanics and ergonomics to reduce musculoskeletal injuries.
- Manage acute pain effectively after injury or surgery to prevent chronicization.
- Treat mood disorders and sleep disturbances early, since they predict chronic pain.
- Stay active and maintain a healthy weight to reduce joint stress and systemic inflammation.
These measures won’t eliminate all pain, but they reduce the chance of it becoming persistent and disabling.
When to Seek Medical Help
Most pain is self-limited, but seek medical attention if pain is severe, sudden, accompanied by neurological deficits (numbness, weakness), fever, unexplained weight loss, or if it disrupts daily life. Early assessment can identify red flags and allow timely interventions.
Questions to Ask Your Clinician
- What type of pain do I have and what’s likely causing it?
- What are the goals of treatment (reduce pain, improve function, both)?
- What are the risks and benefits of recommended treatments?
- How will we know if the plan is working?
- Are there non-drug options I should try?
A shared decision-making approach leads to better outcomes.
Pain Research: Where Science Is Heading
Pain research is increasingly interdisciplinary, combining molecular biology, imaging, psychology, and engineering. Active areas include:
- Identifying biomarkers for different pain mechanisms to tailor treatments.
- Developing safer analgesics that avoid addiction and systemic side effects.
- Refining neuromodulation techniques to target specific circuits.
- Understanding how immune cells and glia in the nervous system contribute to chronic pain.
Progress is steady, and the future holds the promise of more personalized and effective pain care.
Quick Reference Tables
Types of Pain and Typical Features
| Type | Features | Common Treatments |
|---|---|---|
| Nociceptive | Sharp or aching, linked to tissue damage or inflammation | NSAIDs, physical therapy, local interventions |
| Neuropathic | Burning, electric, shooting; follows nerve distribution | Anticonvulsants, antidepressants, topical agents |
| Inflammatory | Warmth, swelling, pain with movement | Anti-inflammatories, disease-modifying agents |
| Centralized (central sensitization) | Widespread pain, heightened sensitivity, fatigue, sleep issues | Multimodal: exercise, CBT, certain meds (SNRIs), sleep optimization |
Pain and Society: The Bigger Picture
Pain has social and economic dimensions. Chronic pain is one of the leading causes of disability worldwide, affecting work, relationships, and mental health. Social support, access to care, and stigma shape outcomes. Policies that improve access to multidisciplinary pain care, mental health services, and safe medications can make a real difference for communities.
A Final Thought Before the Conclusion
If you’re living with pain or caring for someone who is, remember two core truths: pain is real, and pain is treatable. Even when cures aren’t available, suffering can be reduced and function improved. Modern pain care embraces biology, psychology, and social context; it recognizes that healing involves not just tissues but thoughts, habits, and relationships too.
Conclusion
Pain is a multifaceted experience created by interactions between peripheral nerves, spinal circuits, and widespread brain networks that weigh sensation, emotion, memory, and context; understanding pain means recognizing both the biological signals and the mental and social factors that shape them, and effective care combines physical, medical, psychological, and lifestyle strategies to reduce suffering and restore function.